Summary
DOI: 10.1373/clinchem.2018.287136
An 8-year-old boy presented to the emergency department with complaints of intermittent stiffening of his upper and lower limbs.
Student Discussion
Student Discussion Document (pdf)
Tony Huynh1,2,3*† and Urs Wilgen2,3
1Department of Endocrinology and Diabetes, Lady Cilento Children’s Hospital, South Brisbane, Queensland, Australia; 2Department of Chemical Pathology, Pathology Queensland, Herston, Queensland, Australia; 3Faculty of Medicine, The University of Queensland, St. Lucia, Queensland, Australia.
*Address correspondence to this author at: Department of Endocrinology and Diabetes, Queensland Children’s Hospital, South Brisbane QLD 4101, Australia. Fax +61-7-33196492; e-mail [email protected]
Case Description
An 8-year-old boy presented to the emergency department with complaints of intermittent stiffening of his upper and lower limbs. Shortly after his arrival he had a large volume (approximately 500 mL) of nonbilious projectile vomit. He described general weakness and fatigue the previous night and on waking, with no history of headaches, diarrhea, fevers, or other symptoms of infection.
In the past 4 months he had experienced intermittent generalized abdominal pain, nausea, anorexia, vomiting, and mild weight loss (3 kg). He had presented 2 months earlier with vomiting. Investigations including a complete blood count, electrolytes, liver function tests, albumin-corrected calcium, magnesium, and phosphate were within reference intervals at that time. An abdominal ultrasonography was unremarkable. The episodes of vomiting had become increasingly more frequent and forceful. His past medical history was otherwise unremarkable.
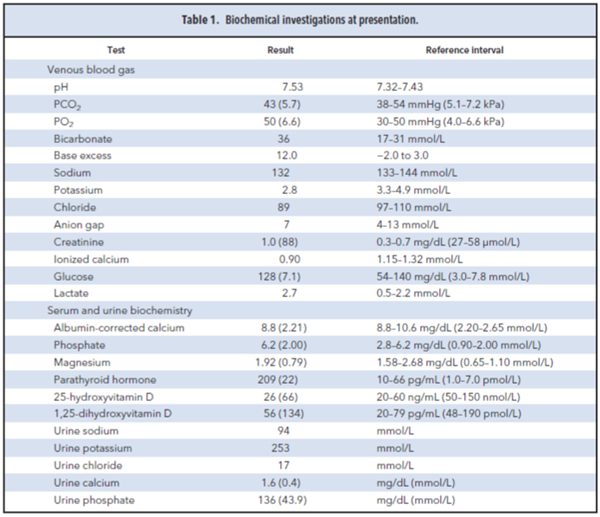
On presentation he was afebrile but tachycardic (pulse rate 156 bpm), tachypneic (respiratory rate 32/min), and mildly hypertensive (bp 125/78 mmHg). He was intermittently drowsy but easily rousable. He was described as having “locked hands and curled toes” consistent with carpopedal spasms and twitching movements of his tongue. He had no focal neurological signs, and his power and reflexes were essentially normal. There were no cardiac murmurs, and his respiratory examination was unremarkable. His abdomen was soft and nontender, with normal bowel sounds. Biochemical testing on presentation showed hypokalemia, hypochloremia, and hyperbicarbonatemia (Table 1). He had evidence of dehydration and prerenal azotemia (increased urea, creatinine, and urate) and normal total protein and albumin. His
liver function tests, lipase, thyroid function tests, albumincorrected calcium, phosphate, and magnesium were normal. An electrocardiogram revealed a prolonged corrected
QT interval (QTc 480 ms). Despite the normal albumin-corrected calcium, the presence of carpopedal spasms and the prolonged QTc interval prompted the collection of a venous blood gas, which revealed hypocalcemia [ionized calcium of 0.90 mmol/L
(reference interval, 1.15–1.32 mmol/L)], a metabolic alkalosis [pH 7.53
(reference interval, 7.32–7.43), bicarbonate 36 mmol/L (reference interval, 17–
31mmol/L)], and PCO2 of 43 mmHg (reference interval, 38–54 mmHg). In the setting
of metabolic alkalosis, the respiratory drive is typically reduced as part of the process of
respiratory compensation, with the rise in PCO2 blunting the rise in pH. The
presence of tachypnea in this patient was thought to be due to hyperventilation related
to anxiety and distress and potentially may have further worsened the alkalosis
and ionized hypocalcemia, leading to acute symptoms.
Questions to Consider
- What are some of the common causes of metabolic alkalosis in pediatric populations?
- What is the clinical significance of urinary chloride concentration in distinguishing among the
causes of metabolic acidosis?
- What is the effect of pH change on the total and ionized calcium concentrations?
Final Publication and Comments
The final published version with discussion and comments from the experts appears
in the April 2019 issue of Clinical Chemistry, approximately 3-4 weeks after the Student Discussion is posted.
Educational Centers
If you are associated with an educational center and would like to receive the cases and
questions 3-4 weeks in advance of publication, please email [email protected].
AACC is pleased to allow free reproduction and distribution of this Clinical Case
Study for personal or classroom discussion use. When photocopying, please make sure
the DOI and copyright notice appear on each copy.
DOI: 10.1373/clinchem.2018.287136
Copyright © 2019 American Association for Clinical Chemistry