Summary
DOI: 10.1373/clinchem.2018.291559
A 21-year-old man presented to the emergency department (ED) with chest pain, worsening shortness of breath, lethargy, nausea, vomiting, and palpitations.
Student Discussion
Student Discussion Document (pdf)
Christopher W. Farnsworth,1* Thomas J. Baranski2
1Department of Pathology and Immunology and 2Department of Medicine, Washington University in St. Louis. St. Louis, MO.
* Address correspondence to this author at: Washington University School of Medicine, 425 S Euclid Ave., Campus Box 8118, St. Louis, MO 63110. Fax 314-362-1461; e-mail [email protected]
Case Description
A 21-year-old man presented to the emergency department (ED) with chest pain, worsening shortness of
breath, lethargy, nausea, vomiting, and palpitations. He presented to another ED the previous day with similar symptoms and was sent home with a diagnosis of anxiety and panic attack. His only relevant past medical history was repaired Chiari malformation. There was no family history of ischemic heart disease. His lipid concentrations were as follows: total cholesterol, 79 mg/dL [2.05 mmol/L; reference interval (ref), <200], HDL cholesterol, 26 mg/dL (0.67 mmol/L; ref, 40–199), LDL cholesterol, 22 mg/dL (1.14 mmol/L; ref, 0–129), triglycerides, 43 mg/dL (0.49 mmol/L; ref, 0–150), and he had a BMI (body mass index) of 29. The patient was otherwise in normal health.
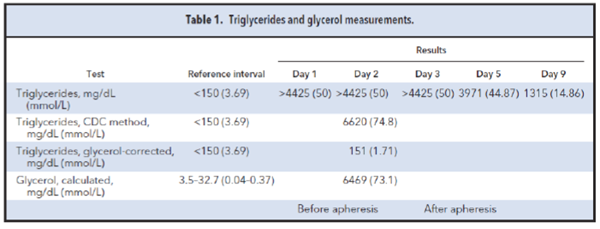
On arrival, his troponin I was 47.94 ng/mL (Siemens Dimension; ref, <0.24). Electrocardiography
(ECG) was performed that revealed sinus tachycardia (140 beats/min) without elevation of ST-segments. As a result, a β blocker was administered for non-ST-elevation myocardial infarction. The patient also developed severe hypoxic respiratory failure with an arterial PO2 of 62 mmHg (ref, 80–100), which required oxygen by nonrebreathing mask at 25 L/min. He was later intubated due to increased respiratory fatigue (respirations 26/min), hypotension (blood pressure 85/57), and increased oxygen requirements. The patient also became oliguric with creatinine increasing to 1.9 mg/dL. He was acidotic, hyperkalemic, and his liver function test results were high (Table 1). There was clinical concern for infection, but all cultures were negative. Furthermore, a urine drug screen, antinuclear antibody, antineutrophil cytoplasmic antibody, and coagulation testing were all normal. Thyroid testing was performed that revealed a thyroid stimulating hormone (TSH) <0.04 mcIU/mL, free thyroxine (FT4) of 0.6 ng/dL (7.7 pmol/L) (ref, 0.7–1.3), and free triiodothyronine (FT3) >20.0 pg/mL (30.8 pmol/L; ref, 2.4–4.2).
Twenty-four hours after admission, bedside ECG demonstrated evidence of acute decompensated heart
failure (HF) with worsening left ventricular dysfunction and an ejection fraction of 21%. Therefore, the β
blocker was stopped and dobutamine was started despite tachycardia. The patient’s heart rate soon
improved to 110, his urine output improved, and troponins trended down. Three days following admission, his symptoms improved dramatically, and extubation was performed; no further complaints of dyspnea or chest pain were received.
Questions to Consider
- What are some causes of decompensated heart failure in otherwise healthy, young individuals?
- What are the indications for thyroid testing in acutely ill patients?
- What are some common causes of acute thyrotoxicosis?
Final Publication and Comments
The final published version with discussion and comments from the experts appears
in the January 2019 issue of Clinical Chemistry, approximately 3-4 weeks after the Student Discussion is posted.
Educational Centers
If you are associated with an educational center and would like to receive the cases and
questions 3-4 weeks in advance of publication, please email [email protected].
AACC is pleased to allow free reproduction and distribution of this Clinical Case
Study for personal or classroom discussion use. When photocopying, please make sure
the DOI and copyright notice appear on each copy.
DOI: 10.1373/clinchem.2018.291559
Copyright © 2019 American Association for Clinical Chemistry