The time to deal with duplicate or nonbeneficial lab orders is at the point of order entry. Once an order is placed and pending in the lab information system (LIS), it is difficult to undo, cancel, or modify. Thus, the electronic medical record (EMR) has great utility in offering real-time decision support and guidance on lab testing for ordering providers.
Our laboratory system has been using the EMR to enhance lab stewardship for several years. One key to our success is having a physician-led department of medical informatics that works closely with our LIS analyst team. Together they review, build, monitor, and update decision support tools that we implemented within our EMR, Epic.
It may feel like we laboratorians spend more time working within the constraints of our EMR and LIS than the systems spend benefiting our workflows. But it doesn’t always have to be that way. Here are four ways we put our EMR to work for our lab stewardship program.
The Answer Is “No”
The most direct measure to tackle unneeded lab testing is a simple ban. Over the years, we have banned, or put “hard stops,” on several tests. Some examples are high-sensitivity C-reactive protein (hsCRP), serum homocysteine, and H. Pylori IgG tests. Instead of simply deleting these order records in Epic, it is preferable to keep an order for a period of time, and have it trigger an alert that informs the clinician who ordered the test why it is no longer available. Figure 1 shows an example.
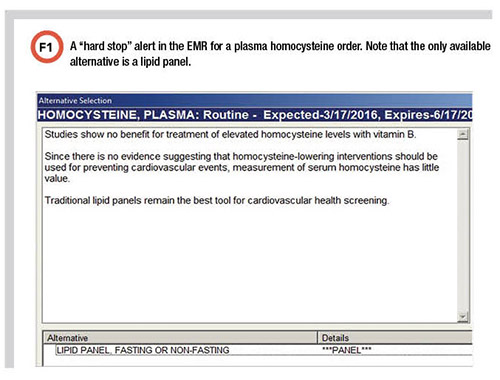
In our system, any lab test, including these banned tests, could still be ordered as a miscellaneous lab test. However, if ordered via this route it would be reviewed and likely not allowed since the test would not be on our approved test formulary.
Reflex Rejects
Creating intelligent reflex options is more difficult, but it is a very useful and clinician-friendly way to reduce wasteful testing. In 2015, Oregon legalized cannabis use. We soon realized that despite THC being legal, we still were confirming the presence of THC in every positive urine drug screen. When a patient admits to using THC, and a positive THC screen result is expected, it does not make sense to send the sample for confirmatory mass spectrometry testing. For this reason, we removed the reflex for THC confirmation from our urine drug screen panels. However, we did create a special urine screen that preserved the THC confirmation reflex but limited this option only to the addiction medicine department. They argued that confirmatory testing was still useful given their unique addiction counseling context.
Another example of adjusting orders to reduce waste was implementing a question-based algorithm for gastroenteritis. We created an algorithm that asks four questions at the time of order entry to determine which test is performed. Based on the answers to questions such as “Has the patient traveled outside the U.S. in the last 30 days?” and “Has the patient been hospitalized or taken antibiotics in the last 30 days?” as well as questions about exposure to shellfish and untreated water, the lab directs the specimen for either C. difficile testing, viral PCR, bacterial PCR, extended bacterial PCR, or parasite PCR testing.
Dealing with Duplicates
Stopping duplicate orders is the Holy Grail of lab stewardship. Epic has a robust duplicate order checking tool that we use for high-volume tests such as complete blood counts (CBC) and the components of a basic metabolic panel. The degree of overrides for these duplicate alerts varies depending on location and environment (such as inpatient versus outpatient settings, and higher versus lower acuity patient demographics). But one can expect to see at least a 20–40% reduction in duplicate orders when duplicate alerts are enabled.
Our lab recently built an alert to curb ordering of differentials. While the CBC itself is commonly overordered, we also have an order for a CBC with differential that is overused. The CBC with differential often requires manual review, which slows down the lab and generates unnecessary charges for the patient. In most cases a simple CBC will suffice. We created an alert that not only informs the provider when the last CBC was ordered, but also automatically changes the next order from a CBC with differential to a simple CBC.
Automatic Notifications
The EMR can also be used to notify ordering clinicians (and the lab), of test interferences. We use an alert in our EMR that fires a notice to the provider when a patient has a serum protein electrophoresis test and has an active prescription for the drug daratumumab. Daratumumab is a monoclonal therapeutic that can present as a band on electrophoresis gels, confounding the measurement of existing monoclonal proteins in gammopathy patients.
We also created an alert for when a patient has their creatinine measured with an Abbott iStat device and the patient has an active prescription for hydroxyurea. Hydroxyurea has a known interference with the iStat creatinine method and will give a falsely elevated result when present in blood or plasma. Although iStats are only used in a few urgent care settings within our system, our EMR is programmed to reconcile the testing method with the patient’s prescriptions and alert the provider and the lab. A message stating that the testing could not proceed at the desired location and needs to be sent to our central lab fires immediately at the time of order entry.
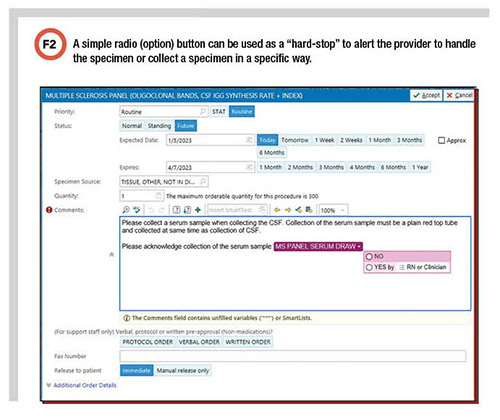
Labs also can add simple checks in the EMR to help ensure the right specimens are collected. We recently included a new prompt when ordering multiple sclerosis oligoclonal band testing. Now, a radio button must be clicked stating that it is a serum specimen. We implemented this after finding that several cerebrospinal fluid samples were sent without the accompanying requisite serum sample.
How to Avoid Too Many Alerts
Lab utilization and stewardship are no longer novel concepts. Over the years, our LIS and Informatics teams have built more than one hundred alerts to guide laboratory test ordering. Now we must be diligent about reviewing the alerts that were put into place at the start of our lab utilization program.
Some of these alerts have now been firing for more than 10 years. One such example is vitamin D. We had an alert aimed at reducing unneeded vitamin D orders. The alert worked well initially and solved the problem we were trying to fix. But alert fatigue happens quickly, and if the alert has served its purpose and is no longer being heeded, it needs to be retired, so we removed it.
Many other useful tips for optimizing (or eradicating) alerts to deal with alert fatigue are available (1). But a good rule of thumb is that a successful alert should lead to an order change at least a third of the time. Moreover, the lab stewardship team should measure the efficacy of alerts annually.
Kevin Foley, PhD, DABCC, MT, SC(ASCP), is director of clinical pathology at Kaiser Permanente NW in Portland, Oregon. +Email: [email protected]
Reference
Jason, C. HER Intelligence. Best Practices to Mitigate EHR Clinical Decision Alert Fatigue. https://ehrintelligence.com/news/best-practices-to-mitigate-ehr-clinical-decision-alert-fatigue (Accessed April 2023).