From ensuring health and safety during the reopening of a professional basketball league during a global pandemic, to allowing women in remote parts of the globe to self-screen for HPV, to improving perioperative pathways for people with diabetes, integrated cross-disciplinary teams continue to show the power of collaboration in improving care and saving lives worldwide. The three initiatives highlighted below are the 2022 top global winners of the UNIVANTS of Healthcare Excellence Awards.
These prestigious global honors were created by Abbott in partnership with AACC and other leading healthcare organizations. The awards recognize teams that collaborate across disciplines to transform healthcare delivery, and ultimately, patient lives. Below we explore the unique achievements of the top winning teams recognized this year.
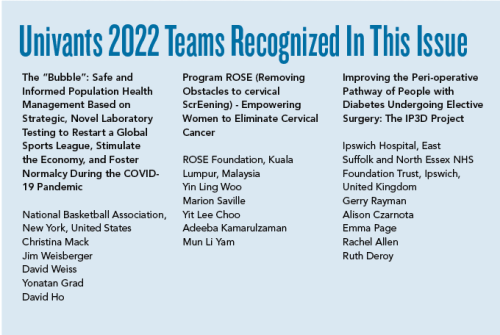
NBA “BUBBLE” SERVES AS MODEL DURING COVID-19 PANDEMIC
Early in 2020, as the world was grappling with how to respond to the Covid-19 pandemic, many sports programs were put on hold. It was at that point, with its season paused, that the National Basketball Association (NBA) decided to take a novel and health-focused approach to keeping players and staff safe while re-starting its season.
The NBA’s closed-campus occupational health program, dubbed the “NBA Bubble,” was operational between July and October 2020. It allowed the NBA to safely re-start, conclude its season, and bring some normalcy to the public during difficult times. More than 300 professional basketball players, 400 team staff, and other NBA league personnel lived and worked in the NBA Bubble.
Christina Mack, an epidemiologist and chief scientific officer, Real World Solutions at IQVIA, a consultant to the NBA, said the top priority in setting up the Bubble was how to do it safely. In partnership with the National Basketball Players Association (NBPA), the NBA convened experts in virology, infectious disease medicine, pathology, lab operations, and infection control. Mack and David Weiss, senior vice president, players matters for the NBA, and others consulted with the team to determine the best way to handle health and safety, while an in-house NBA production and logistics team was charged with setting up operations.
“We weren’t working from a blueprint,” Weiss said. “We had to design everything from scratch.”
Protocols included quarantine upon campus entry, daily PCR testing for thousands of campus residents, indoor masking, physical distancing, comprehensive disinfection procedures, and enhancement of building ventilation. Although these were known infection-control principles, this was an unproven approach not previously attempted at this scale, particularly at this early phase of the pandemic, the group said.
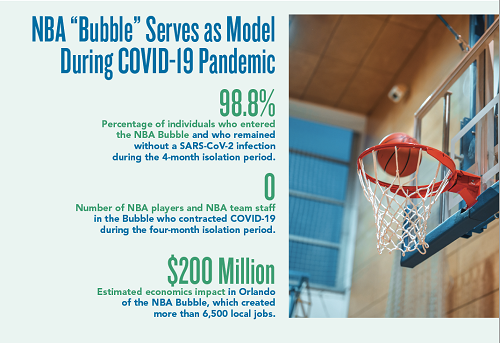
Protocols not only governed the activities of the players and team staff living in the Bubble, but also thousands of vendors who lived off-site and provided transport, security, supplies and inventory management, food preparation, and cleaning services. The testing program for this group was particularly important given their daily risk of exposure within the Orlando community. A temporary healthcare facility was created within the Bubble with an onsite clinic, mobile MRI and CT scanners, mobile dental care, and an on-campus psychologist.
The Bubble had 15 collection sites for nasal/nasopharyngeal samples and four CLIA point-of-care testing (POCT) laboratories for antigen and PCR testing, employing 470 staff to manage collections and logistics from 6 a.m. to midnight, 7 days a week.
The labs verbally communicated POCT results within 20 minutes of collection and performed more than 7,000 POCT tests. In addition, more than 170,000 high-throughput RT-PCR tests were performed by BioReference at a high-complexity CLIA laboratory with locations across the U.S., including one about 75 miles southeast of the Bubble, with sample pickups every 2 hours. The average turn-around-time (TAT) was 9.8 hours after receipt. Overall, turnaround time was consistently less than 24 hours.
Key Clinical Performance Indicators
Of note, 98.8% (3,604 out of 3,648) of the individuals who participated in the NBA Bubble remained without a SARS-CoV-2 infection during the 4-month period, including all players and team staff. Twenty cases were identified during initial quarantine at entry using RT-PCR testing, often before the onset of symptoms. Those individuals were kept isolated at a critical timepoint, and no secondary infections were associated with contact with these individuals. There were no incidences of positive cases among NBA players or team staff once out of quarantine and living in the Bubble.
What’s more, 100% (36 of 36) of previously infected individuals who continued to test positive after recovery did not experience SARS-CoV-2 reinfection nor transmitted the virus to another individual during the 4-month period.
“Working alongside a number of medical and mental health clinicians, and collaborating with world renowned experts in infectious disease, epidemiology and industrial hygiene, we were able to design and apply health and safety protocols to keep Bubble residents as safe as possible during the season restart in Orlando,” said Leroy Sims, MD, head of medical operation for the NBA.
“Further, we created a campus inclusive of on-site medical clinics and advanced imaging capabilities that integrated technology for tracking compliance with daily testing, symptom screening, physical distancing, and contact tracing. Through frequent communication with all residents by means of physical signage, town-hall meetings, emails and in-person briefings, we emphasized compliance with public health measures, which aided in making everyone on campus feel a sense of community and safety amidst the ongoing pandemic.”
Process Attributes
Mack and her team describe the NBA Bubble as highly unique given that it was the first large-scale occupational health operation of its kind during the pandemic to continue operations while preventing the spread of COVID-19.
“The NBA Bubble provided an opportunity for NBA players, staff, and vendors to re-engage in activities far sooner than would have otherwise been possible, allowing the NBA to safely resume sport activities during the height of the pandemic in the summer of 2020,” Mack said.
Implementing the Bubble was demanding work, the team noted, explaining that in addition to creating health and safety protocols, the NBA had to create other crucial elements needed to create a “home” for residents for 4 months in the closed campus environment.
The initiative produced new information about COVID-19 during and after the Bubble that was critical to public health efforts, Mack said. When the NBA Bubble ended in October 2020, the NBA retained strong safety protocols and continued to build on the learnings from the Bubble to mitigate COVID-19 through two subsequent seasons played in team markets.
“The NBA’s learnings and protocols were discussed in real time with public health organizations, including the CDC and FDA, and key findings were extended to other elite sport events and industries,” Mack said. “For example, learnings from the Bubble contributed to the Tokyo Playbook and testing protocols for the Tokyo 2020 Olympics.”
Also notable, Mack said, is that lab-based testing from the Bubble continued through the two subsequent full NBA seasons, creating a unique longitudinal database with insight on transmission, viral trajectories, and vaccine effectiveness. Scientific findings were regularly shared with public-health bodies and other groups working toward virus control to get back to “normal.” Findings also were posted on preprint servers to make the information available in real-time prior to publication in eight high-impact journals, including the New England Journal of Medicine and the Journal of the American Medical Association.
The team credits laboratory medicine as an essential component of the clinical care initiative. Testing protocols evolved during the Bubble based on real-time data, enabling precise decision-making and improvements as more was learned about the virus, as well as diagnostic device effectiveness. While RT-PCR tests approved under the FDA’s emergency use authorization were designed to detect symptomatic infection, test performance in asymptomatic individuals was unknown, and safe clearance protocols for false positive results and individuals who continued to test positive at low levels after recovery were unestablished.
“Within two weeks of program launch, the NBA team evolved protocols to retest all low viral load positive on orthogonal RT-PCR platforms to confirm results, minimizing positive results with very low viral load due to non-infectious particles,” the team said. “Cycle threshold values, inversely correlated to viral load, were added to reports to quantify disease progression and pinpoint post-recovery non-infectious shedding. Decontamination protocols and environmental testing of collection and CLIA testing sites prevented large-scale contamination.”
EMPOWERING WOMEN TO SCREEN FOR HPV THROUGH THE USE OF SELF-COLLECTION
Cervical cancer is the third most common cancer in Malaysian women, but only 25% of eligible women have Pap smears done regularly, due in part to discomfort and inconvenience. In addition, since results can take up to 3 months to be reported, patients often are lost to follow-up and not linked to care. An alternative to Pap smear testing is HPV (Human Papillomavirus) testing, as 99% of cervical cancers are caused by high-risk HPV types.
Program ROSE (Removing Obstacles to Cervical ScrEening) is a primary HPV cervical screening program that incorporates self-sampling and digital technology, ensuring that women who are screened are linked to care. It is an evidence-based, women-centered approach that offers women the choice of using a self-swab to enable high-precision HPV testing, followed by prompt availability of results and navigation of follow-up through the woman’s mobile phone, explained Marion Saville, executive director of the Australian Centre for Prevention of Cervical Cancer (ACPCC), who helped develop the program with Woo Yin Ling, professor of obstetrics and gynecology at the University of Malaya.
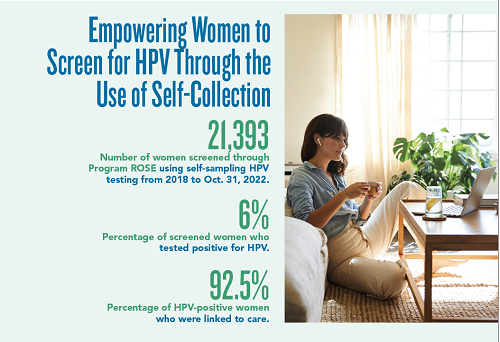
According to Saville, HPV testing provides access to improved diagnostic accuracy, allowing significantly less frequent testing over a Malaysian woman’s lifetime, while still enabling appropriate preventive screening against cervical cancer. With self-sampling, ROSE embodies privacy and dignity, encouraging more women to willingly participate in screening in a timely manner, while the accuracy and reliability of self-swabs for HPV testing provides greater assurance to women, Saville said.
The mobile portal, developed by ACPCC for the ROSE Foundation, facilitates communication and linkage of care for women who test positive, seamlessly navigating women through an otherwise complex and overwhelming health care system. The population registry also enables healthcare professionals to track the progress of every woman screened, regardless of where she was screened.
“This provides a welcome safety net to ensure that women in whom HPV is detected are followed up and managed appropriately, while reducing duplication of services,” Saville commented.
“Program ROSE illustrates the importance of collaborative partnerships and addressing the multi-faceted barriers from policy changes and infrastructure readiness to the implementation of a radically new cervical cancer screening program in communities. The paradigm shift in cervical cancer requires a monumental and concerted effort in educating both the healthcare providers and the public.”
Linking to Care
A total of 21,393 women were screened through Program ROSE using self-sampling HPV testing from 2018 to Oct. 31, 2022. The beneficiaries included underprivileged and underscreened women from more than 12 states in Malaysia. HPV was detected in samples from about 6% of screened women. All HPV-positive women received a referral letter from ROSE for follow-up examination at 26 ROSE-friendly hospitals all over Malaysia, and 92.5% of those women were linked to care.
“The high rate of successful follow-up is a testament to how Program ROSE is able to meet the third pillar of the WHO cervical cancer elimination target – 90% linked to care,” Saville noted. “The linkage to care is usually a weak point of many existing cervical cancer screening programs, which stop at screening without providing post-screening care to those who test positive. Linkage to care is essential to allow early treatment for those who need it and protect women from cervical cancer.”
Almost all women interviewed (99%) said they would repeat the ROSE test again instead of the conventional Pap smear, indicating the self-sampling method is more comfortable and convenient than traditional Pap smears.
Saville added that visiting clinics can be a burdensome chore for many women, as they need to spare time and resources to travel to clinics. In some remote places, traveling to a clinic means traveling for more than 6 hours. Not having to visit a clinic for a test result removes these obstacles, and women are more likely to take up Program ROSE self-sampling HPV test compared to going to clinics for their cervical screening.
Many patients think HPV is a sexually transmitted disease and feel shame, Saville said, noting that proper messaging is important to inform the public and educate them that HPV infection is common and testing positive does not mean they have done anything wrong. Program ROSE is working to educate the public about HPV testing as a way of normalizing this type of testing.
“Cervical cancer is often wrongly associated with sexually transmitted disease and leads to stigma,” says Saville. “In conservative communities, women may avoid coming out for screening due to stigma. Educating not only the women, but the public, will mitigate the stigma associated with cervical cancer and screening, thus enhancing the likelihood of women agreeing to be screened.”
Possible to Replicate
The unique components of Program ROSE do not require heavy investments in infrastructure, according to Saville, who noted that education can be performed using trained volunteers and enhanced with digital materials. Screening can be done in the community where women are most comfortable while communication and delivery of results is digitally enabled.
Because self-sampling removes the need for pelvic examinations to obtain a specimen, this type of program can be scaled up rapidly.
“Program ROSE can be replicated easily,” Saville said. “This is demonstrated in our community outreach programs where women from all different walks of life can execute the program in their community. On a larger scale, ROSE can be implemented in other low- and middle-income countries. The key components of the ROSE approach, including HPV testing, self-sampling, and linkage to care, can be adapted to the needs of diverse communities. These principles underpin the Eliminate Cervical Cancer in the Western Pacific initiative, a philanthropically funded project currently operating in Papua New Guinea and Vanuatu.”
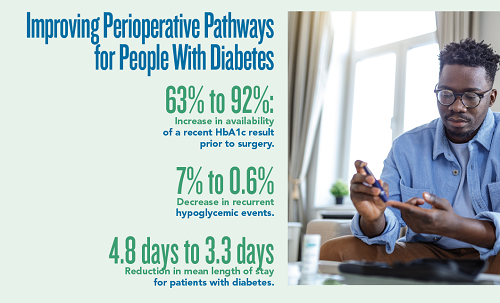
IMPROVING PERIOPERATIVE PATHWAYS OF PEOPLE WITH DIABETES
Elective surgery can be particularly challenging for people with diabetes, with many experiencing anxiety and dissatisfaction with their care. Furthermore, people with diabetes experience higher rates of perioperative mortality, suffer more postoperative complications, have a longer length of stay, and increased readmission rates.
Despite numerous guidelines, there has been little improvement in the perioperative care of people with diabetes, according to Gerry Rayman, a consultant diabetologist at Ipswich Hospital, part of the East Suffolk and North Essex NHS Foundation Trust in the United Kingdom.
To improve the care of patients undergoing elective surgery, Ipswich Hospital formed a diabetes-surgery workgroup. The group developed an initiative, “Improving the Perioperative Pathway of People with Diabetes Project” (IP3D), which included use of a handheld “diabetes perioperative passport” to empower patients throughout their journey, recruitment of surgical diabetes champions, and the roll-out of surgical diabetes study days.
The passport describes what the patients should do to prepare for surgery, including why surgery may be deferred if their HbA1c is elevated, what to do with their medications on the day prior to admission, and what to expect during their stay.
A key component of IP3D was recruiting a perioperative diabetes specialist nurse (DSN), whose role included engaging and educating others involved in the pathway and supporting patients with their diabetes care pre-surgery and throughout the admission, Rayman said.
To determine whether outcomes for patients improved, the group undertook a baseline audit of 185 patients listed for elective surgery between July and December 2017 before starting the program, followed by an audit of 166 patients listed for surgery during implementation (July to December 2018). They measured staff knowledge and patient experience via questionnaires.
Positive Results
Results showed that the availability of recent HbA1c increased from 63% to 92%, which made diabetes more visible and more likely to be taken into account when planning for surgery. The mean HbA1c of those seen for optimizations by the Perioperative DSN significantly decreased from a mean of 9.8% to 7.8%. Recurrent hypoglycemia decreased from 7% to 0.6%, and the mean number of hyperglycemic events per patient dropped almost in half, from 3.0 to 1.7.
In addition, the mean length of stay decreased from 4.8 to 3.3 days. Importantly, this was not associated with an increase in the 30-day readmissions. Post-op complications, including poor wound healing and infections, significantly decreased from 28% to 16%.
“This not only makes for a better patient experience, but also is one of the main contributors to reduced length of stay,” Rayman said. “Reduced complications suggest the patients are experiencing better diabetes care both before and during their hospital admission.”
What’s more, there was a significant increase in staff knowledge and confidence in diabetes management and patient feedback was excellent, Rayman said, adding that the IP3D pathway improved important perioperative outcomes for those with diabetes undergoing elective surgery. Patients reported that the passports given to them at their pre-operative assessment were helpful and informative, and nursing staff used them as an educational tool for their own professional learning and development.
In fact, staff confidence in safely omitting insulin on the day of surgery increased significantly, which ensured that operations were not cancelled at the last minute due to concerns over glycemic control.
In terms of cost savings, a total of 157,000 pounds per year (525 hospital bed-days) was saved due to a 1.5-day reduction in patient length of stay across 350 elective procedures per year.
“This savings more than repays the cost of the intervention without taking into account the additional benefits of improved patient flow and the impact of the reduction in complications on the wider health system,” Rayman said.
While the initiative was initially funded through the hospital’s own diabetes charity funds, the evidence and potential cost savings led to full Trust funding. Subsequently, 10 UK hospitals have introduced IP3D with similar benefits, which indicates that the IP3D pathway is transferable and adaptable.
“With similar outcomes achieved to those that were seen at Ipswich, the pathway has the potential to offer substantial cost savings across the NHS,” Rayman said.
Preparation Key to Implementation
The IP3D program was not difficult to implement, but did require a lot of preparation, including developing the business case for employing the diabetes perioperative nurse, training of the nurse, producing the various tools used and patient experience questionnaires. Rayman noted that systems needed to be in place for extraction of blood glucose and HbA1c data, length of stay, readmission rates, and postoperative complications.
Extracting the capillary blood glucose (CBG) data was automated and provided good insight into the level of glucose control achieved in this group of people with diabetes, Rayman explained. The business informatics team extracted the length of stay and readmission data and formed an important overview of performance. Patient notes were manually audited to ensure pathway compliance with national guidelines, and data was fed back at anesthetic audit meetings.
The IP3D working group, which included representatives from the diabetes inpatient team, preoperative assessment team, pharmacy, and surgical ward staff, met once a month. The laboratory provided two essential biochemical measures that improved the safety of people with diabetes undergoing elective surgery – HbA1c and CBG measures.
“We were able to access HbA1c results prior to referrals and at pre-assessment both before and after introducing IP3D,” Rayman said. “This showed improvement in the various key performance indicators related
to HbA1c.”
The team also used a patient data management system in all clinical areas, including surgical theaters, to measure CBG. These were configured to provide alerts to staff and bedside actions for out-of-range values. In addition, the web link allowed for remote viewing by the diabetes staff to identify patients requiring prompt review of their control, added Rayman.
TRANSFORMING PATIENT LIVES
Each of these initiatives demonstrates the critical role that laboratory medicine plays in improving health outcomes and savings lives throughout the world.
Beyond providing test results, lab experts increasingly take an active role in such integrated teams, offering insight and data vital to their success. And has become clear during the past few years, labs are on the front in helping keep safe during a global pandemic.
The winning teams highlighted above will receive a physical award, plus the exclusive title, “UNIVANTS of Healthcare Excellence Award Winner.” The teams will also be given opportunities to share more about their initiatives, including an invitation to share their best practices at an exclusive leadership forum.
To learn more about UNIVANTS and past award recipients, go to www.univantshce.com. The supplement is also available as a PDF.
Kimberly Scott is a freelance writer who lives in Lewes, Delaware. [email protected]